Leptospirosis Description
Leptospirosis is caused by spiral shaped germs (bacteria) called Leptospira that damage the liver, kidneys and other organs of animals and humans
Leptospirosis as a disease occurs worldwide; with outbreaks mainly occurring after floods
Leptospira, are excreted through urine of infected animals into the environment where it survives for weeks and months.
Leptospirosis Transmission in humans
Agricultural workers and those working with livestock or wild animals are most at risk of leptospirosis.
Leptospira bacteria gets into the body through broken skin (from a cut or scratch) or through the eyes, nose or mouth.
Contact with urine from an infected animal or urine contaminated soil, water or food exposes humans to infection and can survive there for weeks to months
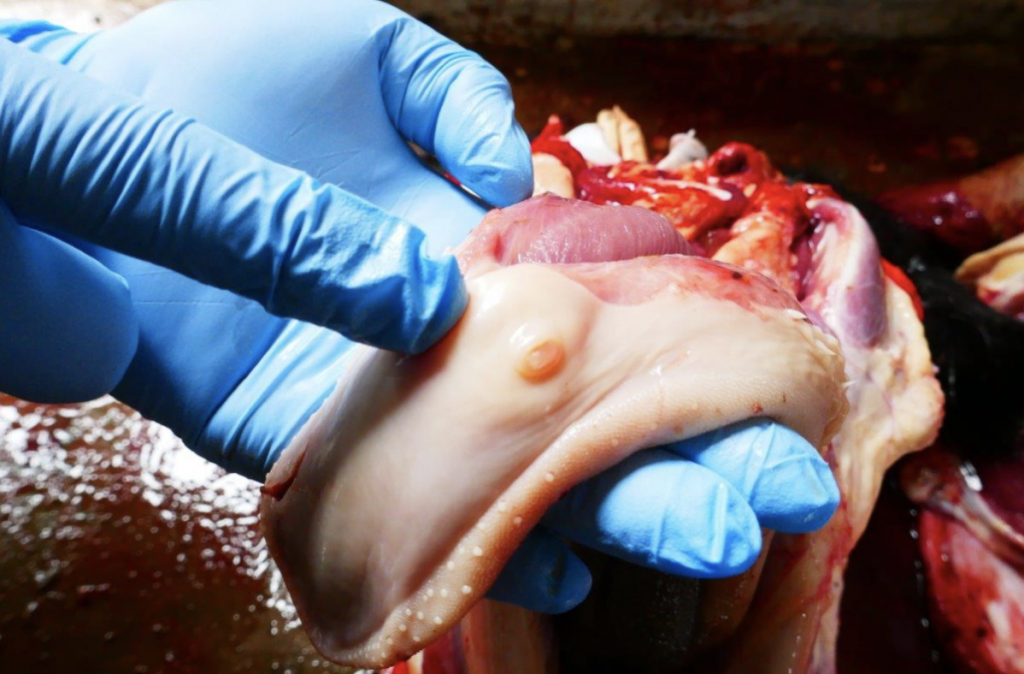
Contact with other body fluids (except saliva), tissues and organs from leptospirosis infected animals can also cause human infection.
Exposure to leptospira contaminated waters i.e. flood waters and rivers cause leptospirosis outbreaks with person to person transmission being rare.
Leptospirosis Symptoms in humans
Leptospirosis in humans present with non-specific symptoms hence can be mistaken for other diseases
Leptospirosis symptoms range from none, mild to severe often due to lack of treatment and death in rare cases.
Mild leptospirosis present with; high fever, headaches, chills, muscle aches, abdominal pain, diarrhea, vomiting, yellowing of the skin and eyes and red eyes.
Severe leptospirosis present with kidney and/or liver damage, infection of the brain and spinal cord, respiratory distress and even death.
Leptospirosis Transmission in animals
Leptospirosis affects cattle, pigs, sheep, goats, rabbits, horses, dogs and rodents.
Leptospirosis is spread through the urine of infected animals, which gets into water or soil and can survive there for weeks to months.
Animals become infected when they come into direct contact with this contaminated water or soil.
The bacteria enter through cuts in the skin or through their eyes, nose or mouth.
Animals can get leptospirosis if their eyes, nose, mouth or broken skin come into contact with infected urine, contaminated soil, water, feed, or bedding
Contact with other unvaccinated livestock and/or rotational grazing may also expose livestock to leptospirosis.
Leptospirosis can also be spread from mother to offspring through the placenta, sometimes through breeding and from a bite by an infected animal.
Eating infected tissues can also expose animals (i.e. dogs) to leptospirosis
Leptospirosis Symptoms in animals
Many animals do not show any signs of illness but they continuously contaminate feed, water, and pastures with the germ causing leptospirosis through urine
General symptoms include: fever, shivering, muscle pain, decreased activity, increased thirst, vomiting, diarrhoea and changes in frequency of urination
Leptospirosis causes bleeding disorders with blood-tinged vomit, urine, stool or saliva; nosebleeds and red spots on gums, other mucous membranes or on skin.
Some animals also develop swollen legs or accumulate excess fluid in their chest or abdomen.
Lactating cows and sheep will have mastitis causing the udder to suddenly become sluggish with resultant milk drop and changes in color and consistency of milk
Abortion may be the only sign of leptospirosis in sheep and goats. Pigs and horses may also experience abortion if infected by this disease.
Leptospirosis causes delivery of dead pigs or poor survival of new born pigs. Kidney damage as a result of infection may also cause failure to thrive in pigs.
In horses, the eye is most commonly affected. The eyelids may be reddened, the horse will be sensitive to light and may blink frequently or clouding of the eye
Leptospirosis Prevention
Do not allow animals to be in contact with contaminated water or soil environments or infected wildlife, especially rodents.
Leptospirosis vaccines are available for pigs, cattle and dogs. These vaccines help to prevent disease severity but may not completely prevent infection.
Always wear gloves, coveralls and gumboots especially if exposed to leptospira contaminated soil, water or infected livestock/other animals (during outbreaks)
Cover any cuts/wounds when handling animals. Avoid direct contact with urine, tissues and organs from potentially infected animals.
Avoid touching eyes, nose and the mouth after handling animals; and do so after proper hand washing.
Practice good hygiene i.e. hand washing with soap and water after handling animals, pets or surfaces that might have pets’ excrement on it.
Keep livestock effluent (faeces and urine) separately, fence or keep stock away from effluent ponds, pits and waterways.
Routine vaccinations for animals whose vaccines are available i.e. dogs and cattle. ST – Ensure completion of treatment regimen for animals undergoing treatment.
Practice good rodent control practices by ensuring that crop and feed stores are rodent free e.g. by making sure no excess feed is lying around.
Leptospirosis Warning
Many animals carry leptospira bacteria but show no clinical signs. It is critical to strictly observe proper hygiene practices especially if an animal is sick e.g. aborted
Lepospirosis is a notifiable disease as it can cause outbreaks. In case of suspicion, report to the nearest health or veterinary department immediately.
If you suspect leptospirosis: (1) In animals – contact your veterinarian immediately; (2) In humans – contact your physician immediately
Content provided by Zoonotic and Emerging Diseases Group (ZED) University of Liverpool , International Livestock Research Institute (ILRI), Zoonoses in Livestock in Kenya (ZooLink)